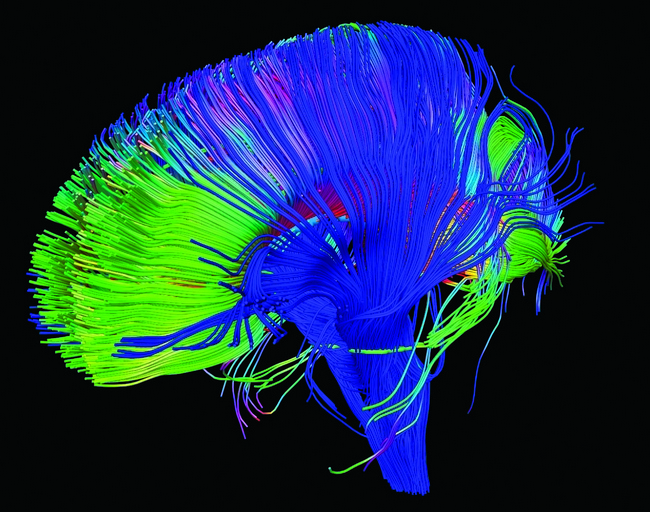
To continue exploring scientific findings on acupuncture, this post will cover its effects on the brain itself and structures of the central nervous system. Primarily through Functional Magnetic Resonance Imaging (fMRI) studies, we know that acupuncture activates specific areas of the brain and deactivates others [1, 2, 3, 4, 5]. Other studies show how these changes affect structures outside the brain influencing multiple body systems through neurotransmitter and hormonal changes.
Activating Resting Brain
The parts of the brain activated during acupuncture overlap with patterns displayed when the brain is at rest [6, 7, 8], going well beyond the somatosensory area that would activate merely from sensations produced by acupuncture. Practically speaking, the effects found in neuroimaging studies is that the parasympathetic, or rest and digest, nervous system takes the reins away from the sympathetic nervous system activated by stress. Parasympathetic activation explains why patients often report both sleeping and digesting better after treatment. More importantly, the changes have been shown to be somewhat point-specific and correspond to areas of the brain with clinical relevance to their reported ancient use.
 For example, a study was performed using the point Gallbladder 34 — a point used since ancient times to treat movement disorders and tremors. This point was found to stimulate the pre-frontal cortex, precentral gyrus, and putamen in patients with Parkinson’s disease. Because the putamen mediates between motor circuits and the basal ganglia, which is degenerated in Parkinson’s, these findings corroborate the specific traditional use for this point [9].
For example, a study was performed using the point Gallbladder 34 — a point used since ancient times to treat movement disorders and tremors. This point was found to stimulate the pre-frontal cortex, precentral gyrus, and putamen in patients with Parkinson’s disease. Because the putamen mediates between motor circuits and the basal ganglia, which is degenerated in Parkinson’s, these findings corroborate the specific traditional use for this point [9].
Notable absences
Generally, there is deactivation in the limbic-paralimbic-neocortical network, or brain areas responsible for pain perception [10]. If the pain is of a muscular or connective tissue origin, as the previous post concluded, acupuncture can also correct the dysfunction causing the pain rather than merely affecting the perception of it. Again, the deactivation pattern is also point-specific.
 For example, in one study, acupuncture was performed at the point Large Intestine 4 in 13 subjects producing prominent deactivation in the nucleus accumbens, amygdala, hippocampus, parahippocampus, hypothalamus, ventral tegmental area, anterior cingulate gyrus, caudate, putamen, temporal pole, and insula in all 11 subjects who experienced ‘acupuncture sensation.’ In marked contrast, signal increases were observed primarily in the somatosensory cortex. Superficial tactile stimulation to the same point elicited signal increases in the somatosensory cortex as expected, but no signal decreases in the aforementioned deep structures [4, 11]. The deactivation of the amygdala and hypothalamus during acupuncture, but not touch, suggests how acupuncture treats major depression and other mood disorders characterized by amygdala hypersensitivity to negative emotional stimuli.
For example, in one study, acupuncture was performed at the point Large Intestine 4 in 13 subjects producing prominent deactivation in the nucleus accumbens, amygdala, hippocampus, parahippocampus, hypothalamus, ventral tegmental area, anterior cingulate gyrus, caudate, putamen, temporal pole, and insula in all 11 subjects who experienced ‘acupuncture sensation.’ In marked contrast, signal increases were observed primarily in the somatosensory cortex. Superficial tactile stimulation to the same point elicited signal increases in the somatosensory cortex as expected, but no signal decreases in the aforementioned deep structures [4, 11]. The deactivation of the amygdala and hypothalamus during acupuncture, but not touch, suggests how acupuncture treats major depression and other mood disorders characterized by amygdala hypersensitivity to negative emotional stimuli.
Beyond the Brain
The limbic structures deactivated are central to regulating emotion, cognition, bio-behavior, endocrine and autonomic nervous functions, and are activated by stress and pain in addition to negative emotions [10]. Deactivating them may allow negative stimuli to roll off one’s back so to speak, and decrease the overall allostatic load caused by stress so that the body can do what it needs to do to heal.
 Another study of acupuncture points Triple Heater 5, Gallbladder 34, and Gallbladder 20 found that these points, traditionally used for the treatment of migraines, activate specific brain regions associated with pain reduction. Specifically, PET-CT neuroimaging revealed “cerebral glucose metabolism changes in pain-related brain regions and reduce(s) intensity of pain” [12]. Similarly, animal data acquired indicate that acupuncture suppresses the synthesis or release of dopamine induced by pain [13], cocaine [14] or alcohol [15]. It would be difficult to chalk up the findings of these studies showing site-specific reactions in the brain and beyond to merely a placebo effect.
Another study of acupuncture points Triple Heater 5, Gallbladder 34, and Gallbladder 20 found that these points, traditionally used for the treatment of migraines, activate specific brain regions associated with pain reduction. Specifically, PET-CT neuroimaging revealed “cerebral glucose metabolism changes in pain-related brain regions and reduce(s) intensity of pain” [12]. Similarly, animal data acquired indicate that acupuncture suppresses the synthesis or release of dopamine induced by pain [13], cocaine [14] or alcohol [15]. It would be difficult to chalk up the findings of these studies showing site-specific reactions in the brain and beyond to merely a placebo effect.
Quality Not Quantity
Returning to the Large Intestine 4 study, the two subjects who experienced pain instead of ‘acupuncture sensation’ exhibited signal increases instead of decreases in the anterior cingulate gyrus, caudate, putamen, anterior thalamus, and posterior insula. This shows that the commonly reported subtle aching, soreness or pressure felt during acupuncture (referred to in this study as ‘acupuncture sensation’) is associated with decreased brain activity in the limbic system and in the default mode network, while sharp pain is generally associated with signal increases in these same regions [4]. Therefore, differences in skill, technique or other differences in methodology may contribute to discrepancies noted in some neuroimaging studies [5, 16, 17].
In conclusion, not only are the effects of acupuncture not produced by manual therapy, they are point specific, and the technique of the acupuncturist is key to eliciting the desired effects within the brain and nervous system. You should not be in ‘pain’ during an acupuncture treatment! I always tell my patients to let me know if for some reason one of the points is uncomfortable or preventing them from relaxing, and I make adjustments accordingly to yield the optimal effect. More studies are needed to yield further insight into the role of acupuncture on the human body and how differences in technique influence its efficacy.
Works cited:
1. Fang SH, Zhang SC, Liu HB. Study on brain responses to acupuncture by functional nuclear magnetic resonance – observations on 10 healthy subjects. Zhongguo Zhong xi yi ze he za zhi. 2006;26:965–968.
2. Fang J, Jin Z, Wang Y, Li K, Kong J, Nixon EE, Zeng Y, Ren Y, Tong H, Wang Y, et al. The salient characteristics of the central effects of acupuncture needling: limbic-paralimbic-neocortical network modulation. Hum Brain Mapp. 2008;30:1196–1206.
3. Napadow V, Dhond RP, Purdon P, Kettner N, Makris N, Kwong KK, Hui KK. Correlating acupuncture FMRI in the human brainstem with heart rate variability. Conf Proc IEEE Eng Med Biol Soc. 2005;5:4496–4499.
4. Wang W, Liu L, Zhi X, Huang JB, Liu DX, Wang H, Kong XQ, Xu HB. Study on the regulatory effect of electro-acupuncture on hegu point (LI4) in cerebral response with functional magnetic resonance imaging. Chin J Integ Med. 2007;13:10–16.
5. Wu MT, Hsieh JC, Xiong J, Yang CF, Pan HB, Chen YC, Tsai G, Rosen BR, Kwong KK. Central nervous pathway for acupuncture stimulation: localization of processing with functional MR imaging of the brain–preliminary experience. Radiology. 1999;212:133–141.
6. Hui KK, Marina O, Claunch JD, Nixon EE, Fang J, Liu J, Li M, Napadow V, Vangel M, Makris N, et al. Acupuncture mobilizes the brain’s default mode and the anti-correlated network in healthy subjects. Brain Res. 2009;1287:84–103.
7. Fox MD, Snyder AZ, Vincent JL, Corbetta M, Van Essen DC, Raichle ME. The human brain is intrinsically organized into dynamic, anti-correlated functional networks. Proc Natl Acad Sci U S A. 2005;102:9673–9678.
8. Fransson P. Spontaneous low-frequency BOLD signal fluctuations: an fMRI investigation of the resting-state default mode of brain function hypothesis. Hum Brain Mapp. 2005;26:15–29.
9. Yeo S, Choe IH, van den Noort M, Bosch P, Jahng GH, Rosen B, Kim SH, Lim S. Acupuncture on GB34 activates the precentral gyrus and prefrontal cortex in Parkinson’s disease. BMC Complement Altern Med. 2014 Sep 15;14:336. doi: 10.1186/1472-6882-14-336.
10. Hui KKS, Marina O, Liu J, Rosen BR, Kwong KK. Acupuncture, the Limbic System, and the Anticorrelated Networks of the Brain. Auton Neurosci. 2010 Oct 28; 157(0): 81–90.
11. Hui KKS, Liu J, Makris N, Gollub RL, Chen AJ, Moore CI, Kennedy DN, Rosen BR, Kwong KK. Acupuncture modulates the limbic system and subcortical gray structures of the human brain: evidence from fMRI studies in normal subjects. Hum Brain Mapp. 2000;9(1):13-25.
12. Yang J, Zeng F, Feng Y, Fang L, Qin W, Liu X, Song W, Xie H, Chen J, Liang F. A PET-CT study on specificity of acupoints through acupuncture treatment on migraine patients. BMC Complement Altern Med. 2012 Aug 15;12:123. doi: 10.1186/1472-6882-12-123.
13. Shi MT, Li L, He GR, Lu GW. Effect of somatosensory stimulation at specific points on levels of monoamines in cerebrospinal fluid. Acta Beijing Second Med Coll. 1986;7:15–18.
14. Yang CH, Shim I, Kim SY. Acupuncture attenuates the neurochemical and behavioral sensitization to repeated DA in cocaine treatment. Abstr Soc Neurosci. 2001;27:228.
15. Yoon SS, Kwon YK, Kim MR, Shim I, Kim KJ, Lee MH, Lee YS, Golden GT, Yang CH. Acupuncture–mediated inhibition of ethanol-induced dopamine release in the rat nucleus accumbens through the GABAB receptor. Neurosci Lett. 2004;369:234–238.
16. Bai L, Qin W, Tian J, Dong M, Pan X, Chen P, Dai J, Yang W, Liu Y. Acupuncture modulates spontaneous activities in the anti-correlated resting brain networks. Brain Res. 2009;1279:37–49.
17. Liu S, Zhou W, Ruan X, Li R, Lee T, Weng X, Hu J, Yang G. Activation of the hypothalamus characterizes the response to acupuncture stimulation in heroin addicts. Neurosci Lett. 2007;421:203–208.